Page 7 - HPP ANTIMICROBIAL GUIDELINE 2018
P. 7
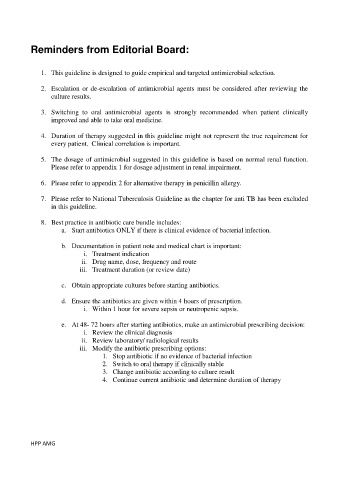
Reminders from Editorial Board:
1. This guideline is designed to guide empirical and targeted antimicrobial selection.
2. Escalation or de-escalation of antimicrobial agents must be considered after reviewing the
culture results.
3. Switching to oral antimicrobial agents is strongly recommended when patient clinically
improved and able to take oral medicine.
4. Duration of therapy suggested in this guideline might not represent the true requirement for
every patient. Clinical correlation is important.
5. The dosage of antimicrobial suggested in this guideline is based on normal renal function.
Please refer to appendix 1 for dosage adjustment in renal impairment.
6. Please refer to appendix 2 for alternative therapy in penicillin allergy.
7. Please refer to National Tuberculosis Guideline as the chapter for anti TB has been excluded
in this guideline.
8. Best practice in antibiotic care bundle includes:
a. Start antibiotics ONLY if there is clinical evidence of bacterial infection.
b. Documentation in patient note and medical chart is important:
i. Treatment indication
ii. Drug name, dose, frequency and route
iii. Treatment duration (or review date)
c. Obtain appropriate cultures before starting antibiotics.
d. Ensure the antibiotics are given within 4 hours of prescription.
i. Within 1 hour for severe sepsis or neutropenic sepsis.
e. At 48- 72 hours after starting antibiotics, make an antimicrobial prescribing decision:
i. Review the clinical diagnosis
ii. Review laboratory/ radiological results
iii. Modify the antibiotic prescribing options:
1. Stop antibiotic if no evidence of bacterial infection
2. Switch to oral therapy if clinically stable
3. Change antibiotic according to culture result
4. Continue current antibiotic and determine duration of therapy
HPP AMG